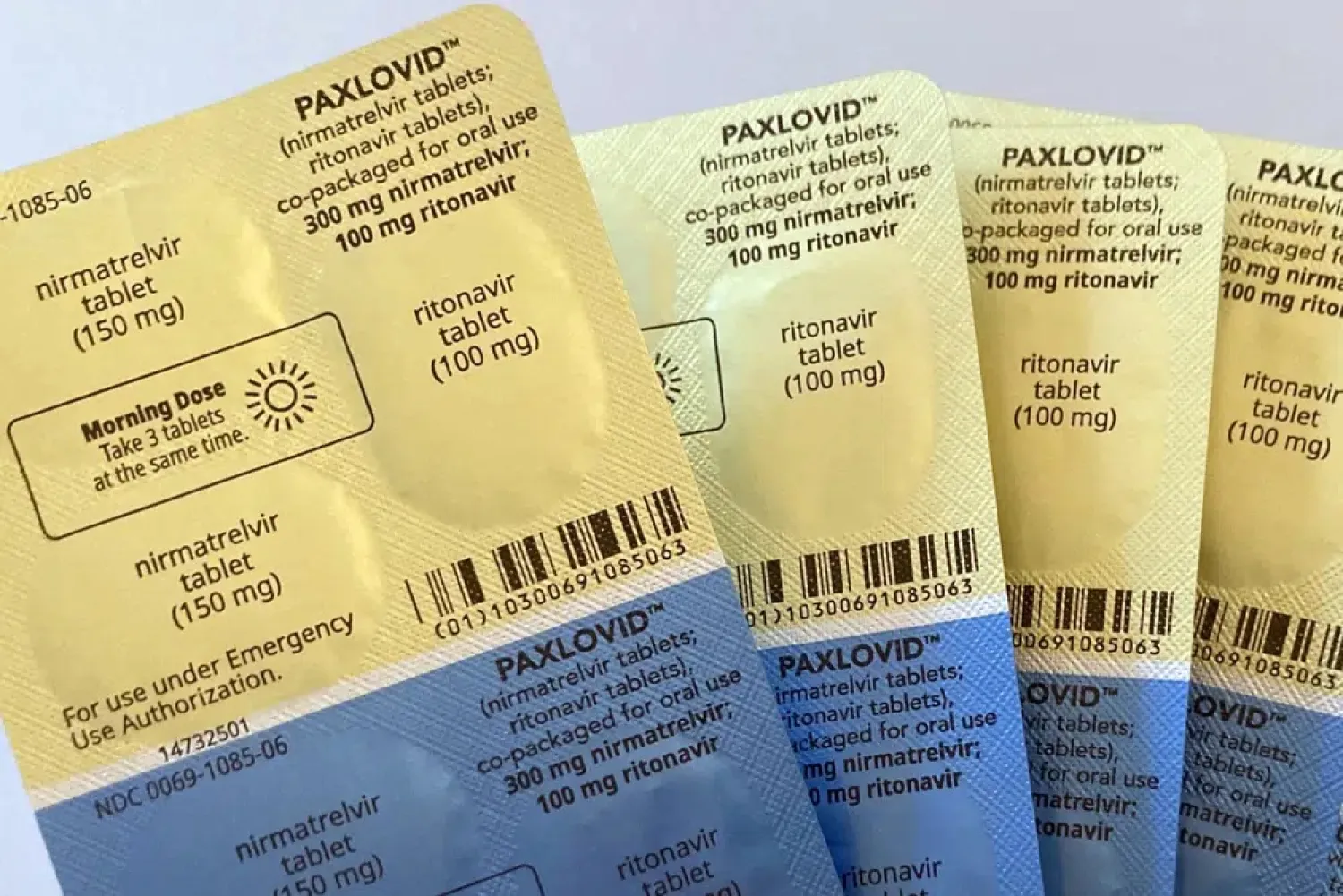
Pfizer’s COVID-19 pill Paxlovid won another vote of confidence from US health advisers Thursday, clearing the way for its full regulatory approval by the Food and Drug Administration.
The medication has been used by millions of Americans since the FDA granted it emergency use authorization in late 2021. The agency has the final say on giving Pfizer’s drug full approval and is expected to decide by May, The Associated Press.
A panel of outside experts voted 16-1 that Paxlovid remains a safe and effective treatment for high-risk adults with COVID-19 who are more likely to face hospitalization and death due to the virus.
“We still have many groups that stand to benefit from Paxlovid, including unvaccinated persons, under-vaccinated persons, the elderly and the immuno-compromised,” said Dr. Richard Murphy of the Department of Veterans Affairs.
The FDA said using Paxlovid in high-risk patients could prevent 1,500 COVID-19 deaths and 13,000 hospitalizations per week.
The panel’s positive vote was widely expected, given that Paxlovid has been the go-to treatment against COVID-19, especially since an entire group of antibody drugs has been sidelined as the virus mutated.
The US continues reporting about 4,000 deaths and 35,000 hospitalizations weekly, the FDA noted.
The agency asked its panel of independent medical experts to address several lingering questions involving Paxlovid, including which people currently benefit from treatment and whether the drug plays a role in cases of COVID-19 rebound.
The panel agreed with assessments by both the FDA and Pfizer that found no clear link between the use of Paxlovid and returning symptoms, but said more information is needed from studies and medical records data. High-profile cases drew attention to the issue last year, including President Joe Biden and first lady Jill Biden.
Between 10% and 16% of patients across multiple Pfizer studies had symptoms return, regardless of whether they’d received Paxlovid or a dummy pill. Such cases “likely reflect natural COVID-19 progression,” the FDA concluded.
The federal government has purchased more than 20 million doses of Paxlovid and encouraged health professionals to prescribe it aggressively to help prevent severe COVID-19. But that’s led to concerns of overprescribing and questions of whether some patients are needlessly getting the drug.
Pfizer originally studied Paxlovid in the highest-risk COVID-19 patients: unvaccinated adults with other health problems and no evidence of prior coronavirus infection. But that doesn’t reflect the US population today, where an estimated 95% of people have protection from at least one vaccine dose, a prior infection or both.
The FDA reviewed Pfizer data showing Paxlovid made no meaningful difference in otherwise healthy adults, whether or not they’d been previously vaccinated.
But when FDA teased out data for high-risk adults — regardless of their vaccination or infection history — Paxlovid still showed a significant benefit, reducing the chance of hospitalization or death between 60% and 85%, depending on individual circumstances. Patients in that group included seniors and those with serious health problems, such as diabetes, obesity, lung disease and immune-system disorders.
With so many different factors, panelists said prescribing Paxlovid will remain a case-by-case decision.
Dr. Sankar Swaminathan of the University of Utah and other panelists stressed the importance of managing potentially dangerous drug interactions between Paxlovid and other commonly used medications.